For all too many of us, cancer hits all too close to home. Unfortunately, we can say the same for the Brit + Co community as a whole. In October 2018, one of our freelance editors Jennifer Garam, 43, was diagnosed with Stage 3 ovarian cancer. In the months since, she has taken control of that diagnosis, battling through many rounds of chemo and an intense surgery. Brooklyn-based Garam shares her story in her own words.
View this post on InstagramA post shared by Jennifer Garam (@jennifergaram) on
Brit + Co: What did life look before your diagnosis?
Jennifer Garam: Up until the day before I was hospitalized and diagnosed with Stage 3 ovarian cancer, I was working as a freelance editor for Brit + Co! Every morning, I’d go to my favorite neighborhood bakery, have a muffin and iced coffee, write in my journal, and then walk to my co-working space to do my editing assignments for the day. I’ve been practicing yoga for 20 years, so about two times a week I’d go to a gentle flow or restorative yoga class. I walk a lot too, but other than that I didn’t do any other forms of exercise or cardio.
I wasn’t the worst eater, but I didn’t really cook or eat particularly healthy food. For dinner, I’d typically have takeout, something simple like pasta and tomato sauce, or one of my favorite go-tos: organic frozen mac and cheese. I ate a lot of sweets, and not a lot of fruits and vegetables, and drank a diet soda every afternoon when I had that 3pm crash. I went through a really stressful, busy period last year when I often ate hot dogs for dinner — which I didn’t know at the time, but now know, are carcinogenic.
Overall, I really struggled with self-care. I tried hard to take care of myself, but my default mode was self-neglect in almost every area of my life, from how I fed myself and ate, to how I dressed and shopped for myself (it would take a long time for me to replace old, worn-out items of clothing or buy things I needed). This also applied to how I related to others. I’d advocate for myself or stand up for myself if I absolutely had to, but internally I’d agonize about it.
B+C: How much did you know about cancer — more specifically, ovarian cancer — prior to your diagnosis? Do you have a family history of either?
JG: I knew very little about cancer in general and nothing at all about ovarian cancer prior to being diagnosed. I didn’t think there was any cancer in my family and didn’t think I was at risk for ever getting it. In some families, all the women have breast cancer, or all the women have ovarian cancer, and that just was not the case in my family — no women had either.
After I was diagnosed, I remembered that I had a maternal uncle and a paternal male cousin who had cancer, but in both instances, it was a long time ago and didn’t seem to have any bearing on me. But then I started digging a little deeper about my family history and discovered that there was some cancer in the family. It was just further back — not my grandparents, but in their generation. And my paternal grandmother died young, at 47, when she was killed by a drunk driver, so I realized that all these years I’d had an incomplete picture of my family medical history because we never knew what diseases she might have developed had she aged.
Shortly after being diagnosed, I had a genetic test done, and the results found that I’m positive for the BRCA1 mutation, which means that it does run in my family. My family members are now in the process of getting their genetic testing done too.
B+C: What was your first indication that there was cause for concern with your health? What did you do next?
JG: I felt fine and thought I was in perfect health. I’d even had my annual GYN exam in mid-May, just four and a half months before being diagnosed with ovarian cancer, and everything was normal.
The last Wednesday in September, I developed chills out of nowhere when I was walking home from the co-working space. That night at home, the chills continued, and I felt feverish and my face was bright red. I also developed stomach pain and a weird shoulder pain which felt connected to my abdominal pain. I Googled the shoulder pain and found some information that indicated it could be related to a gall bladder infection, due to a nerve in the abdominal region that runs up to the shoulder, so that was actually my worst fear of what could be wrong at the time.
The next morning the fever and chills were gone, so I thought I’d just had some kind of 24-hour bug. I had a horrible headache for the next two days, but then that passed. But the stomach pain remained constant, and I was bloated all the time and not just after I ate. Over the weekend, my belly button popped out like a pregnant woman’s, where you could see it through my t-shirt. On Monday and Tuesday, I had some light bladder leakage during the day — it wasn’t like I had to go to the bathroom and couldn’t hold it, it was just that I’d notice that my underwear was a little wet when I went to the bathroom. I thought that because of all the bloating, maybe something was pressing down on my bladder. And part of me thought that, at 43, maybe this was just what it was going to be like from now on — Depends from here until 90.
I have a rule of thumb that if something doesn’t resolve in a week, I go to the doctor, so that Tuesday night, after seven days of having symptoms, I went to urgent care. They thought it was gastritis or colitis and gave me an antacid and an antispasmodic medication, and told me that if I didn’t feel better in three days I should get a CAT scan.
The next morning, I woke up and realized I had wet the bed overnight. This scared me and I knew something was wrong. I knew I had to do something but even so, when I called my mom crying, I told her I wanted to wait until Friday to get a CAT scan because I didn’t work on Fridays and it would be easier to deal with it then than on a workday. “A few days isn’t going to make a difference,” I said. She pushed me to do something about it immediately and not wait.
I called urgent care and they got me in for a CAT scan right away that morning. I still didn’t think it was going to turn out to be anything that serious, so I was emailing my boss at Brit + Co that I was getting a CAT scan and I’d be online for work in the afternoon. That sounds so dramatic, I’d thought, as I read over the email before sending it. I almost added “It’s probably nothing,” but something stopped me from writing that because I really didn’t know.
B+C: Describe the experience of receiving your diagnosis. Do you remember your first thought? What did you do for the rest of the day?
JG: I was supposed to wait at the radiology facility for the CAT scan results, and was told that the radiologist would call urgent care with the results and then urgent care would call me there to tell me over the phone. I was sitting in the waiting area when the women at the front desk told me I had to go straight to urgent care to get the results in person, and that’s when I got really scared and knew that it was serious, and I started crying as I was walking to the subway.
At urgent care, they went over my CAT scan results with me and told me that I had masses on both ovaries, fluid in my abdomen, and lymph node involvement, and these were all markers of ovarian cancer, and that I also had a tumor near my liver. The doctor told me that I had to go to the emergency room for a full work-up IMMEDIATELY, and he even typed “immediately” in all caps in my discharge report.
When I left urgent care, I started calling my family to tell them what was happening. I went to the ER right away, and I was by myself at that point, and when I checked in, I started crying again and the woman who worked there came out from behind the desk and hugged me. I was there by myself for a few hours, and then my mom, my dad and his wife, and one of my close friends got there, and my mom and my friend stayed until midnight, until they knew I was settled in the room I’d be in for the night.
I don’t remember what my first thought was — it all happened so fast and I think I was in shock those first few days.
B+C: What was the next step after your diagnosis? What treatments did you discuss or plan for?
JG: It actually took a few days to get an official diagnosis. I was in the ER for about 24 hours and then admitted to the hospital, and I was in the hospital for a week. When I was in the ER I had more tests done — a blood test and a pelvic exam. I never thought that this was going to turn out to be something else, because every test result came back showing signs of ovarian cancer. For the blood test that showed a marker of cancer, my level was exponentially higher than the norm. And in the pelvic exam, my doctor told me that he could feel the masses. A biopsy is needed to confirm a cancer diagnosis though, and that Friday I had a laparoscopic biopsy, and I got my official diagnosis first thing on Saturday morning.
The most terrifying time was those first few days, when I knew I had ovarian cancer but I didn’t know how advanced it was and what stage it was, and what my prognosis was. That first night, in the ER, I had a private room because I was a GYN patient, but there was no bed so I slept on a GYN exam table. In the middle of the night, I just lied there awake and thought, “Am I going to die now? Is my life over? I’m 43. Is this it for me?”
Knowing the concrete details dissipated that fear. When I got my diagnosis that Saturday morning of Stage 3 ovarian cancer, my doctor also laid out my treatment plan. I’d have nine consecutive weeks of chemo to shrink the cancer before surgery, followed by major surgery to remove the organs affected by the cancer (this wound up being a hysterectomy and oophorectomy, as well as having my appendix removed), and then nine more weeks of weekly chemo.
I opted to have a port implanted for chemo rather than receive it via IV, so I had that surgery to have the port implanted on Monday, and then I started chemo in the hospital on Tuesday night and was released from the hospital that Wednesday.
B+C: After your diagnosis, what resources did you use to learn more about ovarian cancer? Who did you talk to? What did you read?
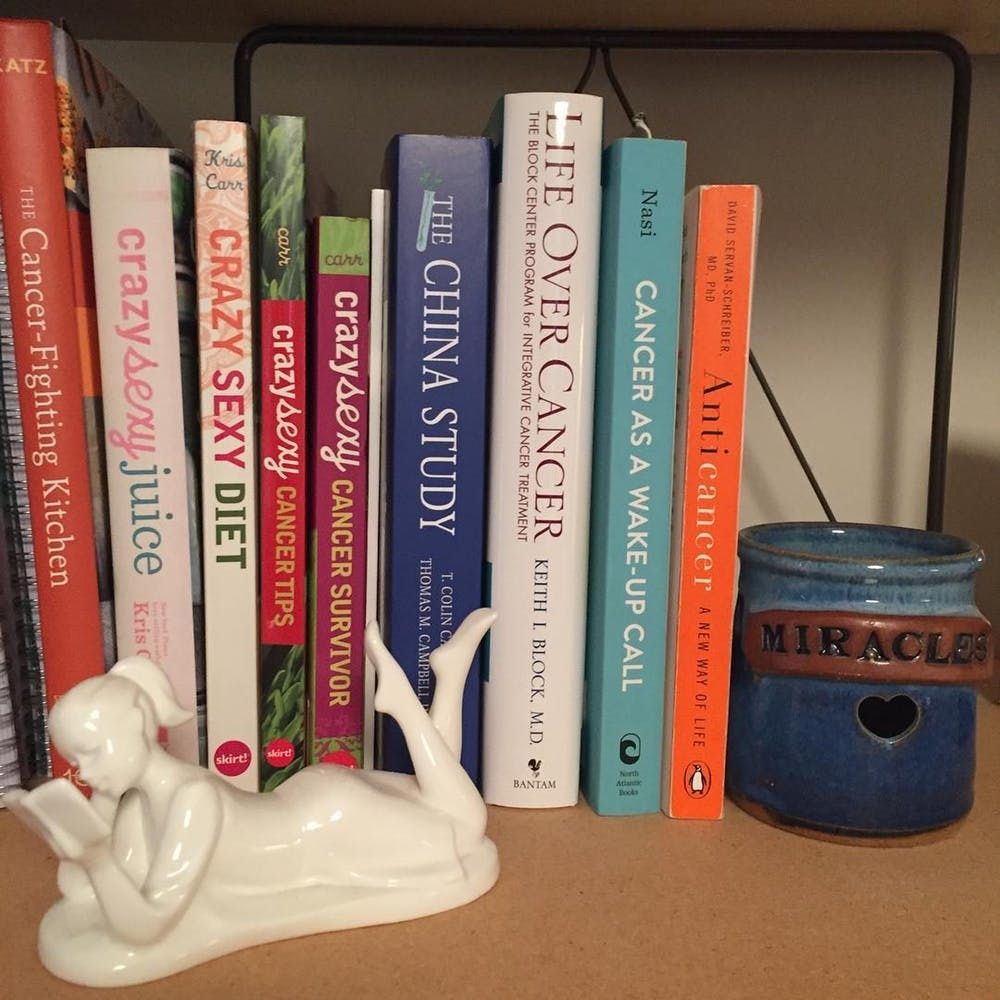
JG: Educating and informing myself about ovarian cancer has definitely been very important to me, and it’s empowering to learn about the disease and the ways I can participate in my own treatment and healing. The first book I read, about six weeks after my diagnosis, was Crazy Sexy Cancer Tips by Kris Carr, which a friend of mine who’s a cancer survivor sent me. Reading that was a turning point for me, because Carr’s writing is so upbeat, positive, and empowering, and my mindset was going in that direction, but I think that book really solidified that positive outlook for me. Since then, I’ve read Crazy Sexy Diet and Crazy Sexy Cancer Survivor by Kris Carr, Anticancer by David Servan-Schreiber, MD, PhD, and Cancer as a Wake-Up Call by M. Laura Nasi, MD, and I’m currently reading Life Over Cancer by Keith I. Block, MD.
I also watched some documentaries about cancer, health, disease, and nutrition: The C Word, Forks Over Knives, and What the Health.
I haven’t yet found a cancer support group I like, but I’ve assembled my own support network of young women cancer survivors I know — some of whom live close by and some of whom are out of state — whom I periodically reach out to for support or with questions, to hear about their experiences with cancer, or to have a meltdown to. That has been so helpful, to have women around my age who have gone through something similar, to talk to and lean on in the tougher moments.
B+C: Could you share more about the treatments you’ve undergone so far? Why did you elect to go this route and how did it feel going through each one?
JG: So far, I’ve done the first nine-week course of chemo, and then I had five weeks off before surgery to rebuild my immune system. In early January, I had the surgery, followed by a month of recovery before resuming chemotherapy. As of this writing, I’ve done three of the nine second-round chemo sessions.
My doctor is incredible and I trust him completely, so I just followed the treatment plan he proposed. That doesn’t mean I haven’t asked questions and tried to understand what was happening — I ask a lot of questions and take a lot of notes, and I’m very involved in knowing what is happening and why every step of the way.
Each new phase and unknown has been scary, but then as I get into a routine, that fear goes away. Chemo was really scary at first, but then I got into a groove with it. I broke down each weekly appointment into three two-hour shifts and created a Google doc spreadsheet for sign-ups, and I have a group of about five or six friends who, between all of them, have covered all my chemo shifts. I now refer to them as my Chemo Squad. My hair fell out from chemo so I got my head shaved, and then it grew back a little but is going to fall out again now that I’m back at chemo, so I’m planning to make another trip to my hairdresser soon. I have some side effects, like fatigue, nausea, and loss of appetite, but at this point, it’s pretty predictable when those will hit during the cycle, so I can plan for it by not making plans those days and staying home and resting.
After the first nine-week round of chemo, I had a PET scan to see if the chemo was working and if the tumors had shrunk enough for me to have surgery. That experience, and waiting for those results, was terrifying, and I had a meltdown to several of my young women cancer survivor friends who all totally understood what that was like to go through. Getting the surgery was terrifying, and I was lying on the operating table crying before I went under. And afterward, it was excruciatingly painful for a little while. But I got through that, with the help of some very strong pain meds that first week, and now that pain has faded to soreness that I only occasionally notice.
B+C: How has your life and routine changed since your diagnosis? What are you doing between treatments to try to rebuild your physical strength?
JG: My life has changed completely. I’m not working so I can focus all of my energy on my health, treatment, and healing. Whereas I used to struggle with self-care, I no longer do, and my most important priority is taking excellent, loving care of myself. I read up on nutrition and see a nutritionist who’s affiliated with my hospital and works with cancer patients. I taught myself to cook and I now eat healthy meals — and no soda or highly processed, packaged food! I also find it easier to stand up for myself now, and don’t feel any internal distress in doing so. I don’t feel a compulsion to people-please anymore because it’s clear to me that the most important and necessary thing is to take care of myself.
As far as building up my physical strength, a few weeks before my surgery I joined a gym and was doing 10-15 minutes of cardio on the elliptical and a little weight lifting. At that time, I also started going to yoga again, after not having gone since my diagnosis, and I found a Yoga4Cancer class that was offered in my neighborhood. I couldn’t exercise while I was recovering from surgery, but last week my doctor cleared me to go back to all forms of exercise, so I’m going to return to the gym and yoga classes.
View this post on InstagramA post shared by Jennifer Garam (@jennifergaram) on
B+C: What’s next in your journey?
JG: As of this writing, I have six more weeks left of chemo. Because I’m BRCA1 positive, I’m also at high risk for breast cancer, so I need to be closely monitored by a breast specialist and have mammograms and breast MRIs (alternating) every six months. I had my first appointment with a breast doctor right before my surgery for ovarian cancer, and she recommended that I have a prophylactic double mastectomy within the next two years. So that’s something I’ll need to consider, but I want to get through my treatment for ovarian cancer first before I make a decision about that.
View this post on InstagramA post shared by Jennifer Garam (@jennifergaram) on
B+C: What have you learned from this experience? What have you learned about yourself?
JG: I have learned A LOT! I’ve learned how much love, kindness, and generosity there is in the world. I have such a tremendous community of friends, family, neighbors, and even people I hardly know who have done so much to help and support me, so often and in so many different ways. For years, I’ve struggled with persistent feelings of loneliness and isolation, and my experience having cancer has shown me that I’m not alone, and I feel more loved and connected than I ever have.
Most importantly, I’ve learned how strong I am. I had no idea that I had this incredible inner strength until I had to face this incredible challenge.
View this post on InstagramA post shared by Jennifer Garam (@jennifergaram) on
B+C: How are you using social media to share your story?
JG: After the shock wore off and I was starting to get acclimated to my new reality, about two and a half weeks after I was released from the hospital in October, I started posting about my cancer diagnosis on Instagram and Facebook. As a writer, I’ve always used writing to heal myself and help others by sharing my experiences and struggles so people going through similar things would know that they’re not alone. Posting on social media about my experiences with ovarian cancer — expressing myself and letting others know what I’m thinking, feeling, and going through — feels very therapeutic to me. And I want people to know what it’s really like to be diagnosed with cancer and undergo treatment for it. In our society, there’s a lot we don’t talk about or show when it comes to illness, and then we don’t know what it’s like to go through an experience like this and the not knowing only adds to the fear. So I want to show it all to dispel that mystery, and hopefully help other people who are going through treatment for cancer, and raise awareness about ovarian cancer for all women.
B+C: What advice would you give women in terms of getting educated about the risk factors for and symptoms of ovarian cancer? What do they need to know?
JG: Well, first of all, they need to know that the symptoms for ovarian cancer are very vague and nonspecific, and could be attributed to anything — or even nothing. According to the American Cancer Society, some of the symptoms include bloating, abdominal pain, and urinary issues such as frequency or urgency. Also, ovarian cancer tends to be asymptomatic in Stages 1 and 2, so it’s often not detected until it’s in the later stages.
My advice would be to read up on all the symptoms of ovarian cancer and pay close attention to your body. If something feels wrong, or is out of the norm, see a doctor. And make sure you get the care and tests you need in an expeditious way, even if it means you have to challenge what your doctors say and advocate for yourself. I’ve heard stories about women who weren’t feeling well for months but ignored their symptoms or didn’t want to deal with it, so they put off going to the doctor. And stories of women who brought up their concerns to their doctor multiple times over a period of months but were continually dismissed, or cases where the necessary tests took a long time to schedule. In my case, when I first went to urgent care I was literally told, “This is nothing serious,” and that it was gastritis or colitis. But I trusted my feeling that something was really wrong when I woke up to having wet the bed, so I called them the next morning and luckily, they caught my ovarian cancer very quickly, about 18 hours after my initial doctor’s appointment.
Lastly, ask your family members if there’s a family history of breast or ovarian cancer, and really dig deep. If you uncover a history of breast or ovarian cancer, and believe that you might be at risk, look into talking to a genetic counselor and getting genetic testing done.
B+C: What do you think is the biggest misconception about cancer, specifically ovarian cancer?
JG: I think the biggest misconception about ovarian cancer is that there’s a screening test for it or that a Pap smear will detect it — there’s not and it won’t. And the biggest misconception about cancer, I think, is that it’s all gloom and doom. It can definitely be brutal; at times, it’s terrifying, mentally and emotionally harrowing, and physically painful. But in the five months since being diagnosed, I’ve also experienced so much joy and love, and connection with others. I have a much greater sense of purpose now, and a deeper sense of meaning. I’ve learned what’s truly important in life and I can see so clearly what’s not, and I’ve discovered my own inner strength and ability to take care of myself. I want to overcome, heal from, and fully recover from this disease. But because of the many, profound ways that this diagnosis has changed my life, and the better, happier, healthier path it’s set me on, I feel that in the bigger picture, getting cancer is the best thing that’s ever happened to me.
Continue following Jennifer’s story and share your love @jennifergaram. Support her recovery on GoFundMe.
Brit + Co may at times use affiliate links to promote products sold by others, but always offers genuine editorial recommendations.